Why Lung Health Matters on World MS Day – And Every Day
Each year on May 30, the world unites to recognise World MS Day – a powerful movement that brings together the global Multiple Sclerosis (MS)
With all of the bush fires around the East Coast, and many people have experienced the effects of smoke inhalation. It is important to understand what is happening in our lungs, how the lungs defend against this and what the potential short and long term damage may be and what you can do about it.
To gain a better understanding of what happens in the lungs when smoke enters the lungs, it is essential to understand what is happening in our lungs, how they defend against this type of invasion and what we need to do to reduce the effects of any potential short and long term damage.
How the lungs defend themselves is the part of the difference between asthma attack symptoms and respiratory attack symptoms they may feel the same, there is a key difference.
As explained in a previous article “Mystery of How Eating Causes Asthma Attacks”, the way an asthmatic reacts to different types of foreign particles and this is explained further in the section “What is the Difference Between Normal Defense and Asthmatic Defense?”.
In the article below, I will explain what the respiratory response is to excessive smoke, the different phases and what the effects are.
Respiratory Response to Excess Smoke and Foreign Particles
The airways have an efficient mechanism called the Mucociliary Escalatory. This includes a combination of hairs on the airway walls called cilia. This mechanism captures and removes up to 90% of foreign particles from the lungs.
When a large number of particles enter the lungs, initially the mucociliary escalator works as normal and can clear these particles efficiently. But as the number of particles increases and become more consistent (which is the case with medium to long term exposure to bush fire smoke), the following steps occur.
Step 1 – When Mucus Becomes Contaminated
The smoke starts building up in the mucus, changing colour. Over time, some of these particles may reach the airway walls, also known as the epithelium (i.e. skin cells), causing the lungs to triggers Step 2.
Step 2 – Cough Mechanism
When the airway walls are agitated by the foreign particles, we have a more explosive defence mechanism called a cough. This can be either instigated manually by ourselves or as a reflex by our body.
The cough occurs by combining expiration, where the diaphragm starts expanding and attempting to push the air from our lungs, while the vocal closes up, stopping the air from escaping. This causes the pressure in the lungs to build up until eventually, the vocal cords open up, and the air explodes from the lungs in an explosive release of air.
The cough is usually employed to assist in the following:
If the agitation of the airway walls continues and the particles aren’t cleared, then Step 3 is triggered.
Step 3 – Respiratory Immune System Response
The consistent agitation and invasion of the particles onto and into the airway walls (epithelium), causes the following 2 processes to occur:
Hypersecretion of mucus – This is a medical term of simply saying that the mucus becomes thicker when changing its properties and the amount of mucus is increased, thus providing a thicker barrier against the foreign particles. This is an attempt to stop any further particles from reaching the airway walls and reduce agitation and/or infection,
This works well during a short term attack but may lead to mucus dysfunction if the invasion of foreign particles lasts for a medium to long time period.
Inflammation of the Airway Walls – This is how the airway walls help to clear the foreign particles, bacteria, etc.… which have already made it through the mucus and into the tissue of the airways. The blood vessels of airway walls release blood into the tissue called inflammation (which causes expansion of the tissue). This allows the white blood cells, from the immune system, to attack and digest the particles, helping to clear them from the area as quickly as possible.
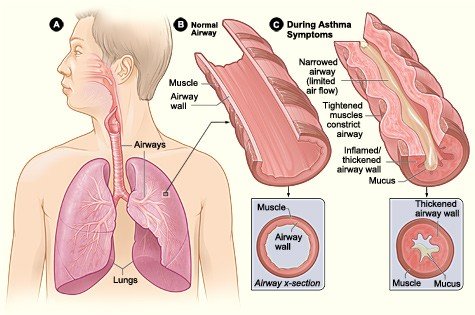
Difference Between This Process and Asthma Attack.
The major difference between a respiratory response compared to an asthma attack is the 3rd type of immune system response, bronchoconstriction.
Bronchoconstriction is a part of the immune system’s response to a parasitic or allergen invasion of the lungs, digestive system or any area which uses a mucociliary escalator as a defence against foreign particles. This includes most parts of the body which have direct exposure to air.
Bronchoconstriction, or also known as bronchospasm is a spasming of the muscles around the airways which helps amplify the cough mechanism in an attempt to expel parasites from the body as fast as possible. Parasites secrete enzymes, proteins and anti-enzymes to break down the bond between the epithelium cells (skin cells) of the lungs. This allows the parasite to feed on the blood secreted from in between the skin cells.
This process doesn’t occur for normal smoke as there aren’t any enzymes, proteins and anti-enzymes in normal smoke.
If you experience long term exposure to smoke, then your lungs become filled with smoke particles, and this may lead to smoke particles going into the alveoli (air sacs where the gas transfer occurs).
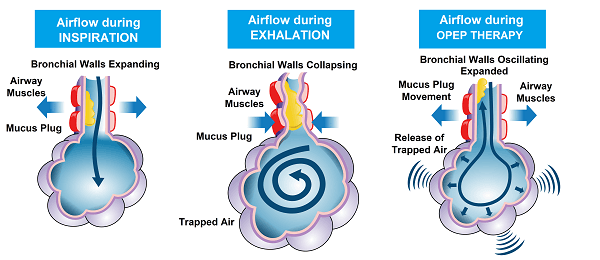
This, in turn, may lead to inflammation of the alveoli, which includes an immune defence of inflammation of the air sacs. This is where the blood vessels of the air sacs open up and bleeding into the alveoli, helping the white blood cells to fight and digest the smoke particles. This can also lead to mucus plugging and inflammation leading to air trapping in the alveolar.
The other issues which may be faced in the airways are that the lungs may develop structural defects of the cilia and epithelium (skin cells). This may lead to an extended length of time for which deposited particles stay in the airways.
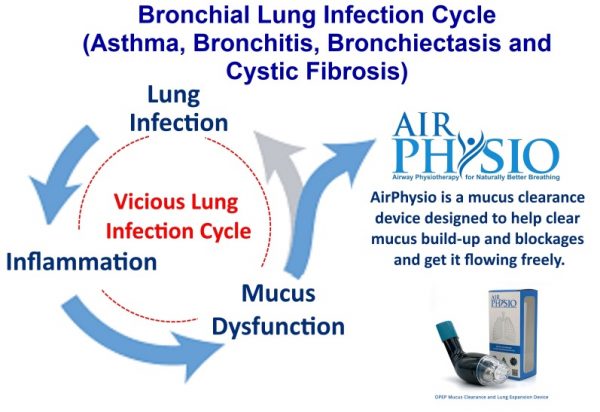
This may cause a longer period of exposure to harmful airborne particulate matter, occupational dust, traffic exhaust and smoke. This creates a vicious cycle of events where the particles are deposited in the airways, they may cause further infection, inflammation and excess mucus to become released.
This, in turn, may lead to mucus dysfunction with the release and buildup of further mucus, causing further infection, inflammation and excess mucus to become released, and the cycle goes on. This may lead to medium to long term damage to the lungs.
So what does this mean?
This means that where a healthy firefighter may be able to have a break for at least 3 hours to assist with removal of up to 49% of the smoke particles, a firefighter with a respiratory condition should have a break of at least 17 hours to assist with the removal of up to 42% of the smoke particles.
What Can Be Done to Help Stop Further Damage?
Like everything, the first step is to stop the source of the problem, which is causing the damage in the first place. This will help the cleaning and healing process to start by allowing the lungs to do what they need to do, i.e. to maintain optimal hygiene and repair the damage.
So to help the body to start the cleaning process, then you need to do the following:
The body is amazing and can cope with a number of extreme conditions, but it is important to not overexpose the lungs to an excess amount of smoke as it may lead to medium to long term damage. It is also important to understand that unless the smoke has chemicals in it which induce an asthma attack, then smoke normally induces a respiratory response to the smoke, rather than an asthma response and that the treatments are usually different. So understanding what happens and why are important for understanding how your body reacts to different particles. The points mentioned above will assist in helping your body to cope better with excessive smoke, while also helping your lungs to expel foreign particles, excessive contaminated mucus and maintain optimal lung capacity.
References
1. Alvaro A. Cruz, MD,a,b Philip J. Cooper, MD, PhD,b,c,d Camila A. Figueiredo, PhD,b,e Neuza M. Alcantara-Neves, MD, PhD,b,e Laura C. Rodrigues, MD, PhD,b,f and Mauricio L. Barreto, MD, PhDb,g Global issues in allergy and immunology: Parasitic infections and allergy, J ALLERGY CLIN IMMUNOL VOLUME 140, NUMBER 5, NOVEMBER 2017 https://www.jacionline.org/article/S0091-6749(17)31509-9/pdf2. Steven A. Saenz, Mark C. Siracusa, Jacqueline G. Perrigoue, Sean P. Spencer, Joseph F. Urban Jr, Joel E. Tocker, Alison L. Budelsky, Melanie A. Kleinschek, Robert A. Kastelein, Taku Kambayashi, Avinash Bhandoola & David Artis. IL25 elicits a multipotent progenitor cell population that promotes TH2 cytokine responses. Nature, 2010; DOI: 10.1038/nature089013. Manoel MedeirosJrMDa, Joanemile P.FigueiredoMDa, Maria C.AlmeidaMDa, Maria AnaliaMatosMDa, Maria I.AraújoMD, PhDadAlvaro A.CruzMD, PhDaAjax M.AttaMD, PhDcMarco Antonio V.RegoMD, PhDbAmélia R.de JesusMD, PhDaErnesto A.TaketomiMD, PhDeEdgar M.CarvalhoMD, PhDad, Schistosoma mansoni infection is associated with a reduced course of asthma, The Journal of Allergy and Clinical Immunology May 2003 Volume 111, Issue 5, Page 947-951 https://www.jacionline.org/article/S0091-6749(03)80119-7/fulltext4. Julian Hopkin, Immune and genetic aspects of asthma, allergy and parasitic worm infections: evolutionary links, Institute of Life Science, School of Medicine, Swansea University, 08 April 2009 https://doi.org/10.1111/j.1365-3024.2009.01104.x Scheuch, G., Kohlhaufl, M., Moller, W., Brand, P., Meyer, T., Haussinger, K.,… Heyder, J. (2008). Particle clearance from the airways of subjects with bronchial hyperresponsiveness and with chronic obstructive pulmonary disease. Experimental Lung Research, 34, 531-549. doi:10.1080/019021408023417105. Möller, W., Häußinger, K., Ziegler-Heitbrock, L., & Heyder, J. (2006). Mucociliary and long-term particle clearance in airways of patients with immotile cilia. Respiratory Research, 7(10), 1-8. doi:10.1186/1465-9921-7-106. Brown, J. S., Zeman, K. L. & Bennett, W. D. (2002). Ultrafine particle deposition and clearance in the healthy and obstructed lung. American Journal of Respiratory and Critical Care Medicine, 166, 1240–1247. doi:10.1164/rccm.200205-399OC7. Osadnik, C.R., C.F. McDonald, B.R. Miller, C.J. Hill, B. Tarrant, R. Steward, C. Chao, N. Stodden, C.C. Oliveira, N. Gagliardi, and A.E. Holland, The effect of positive expiratory pressure (PEP) therapy on symptoms, quality of life and incidence of re-exacerbation in patients with acute exacerbations of chronic obstructive pulmonary disease: a multicentre, randomised controlled trial. Thorax, 2014. 69(2): p. 137-43.8. Forbes, L., Kapetanakis, V., Rudnicka, A., Cook, D., Bush, T., Stedman, J.,… Anderson, J. (2009). Chronic exposure to outdoor air pollution and lung function in adults. Thorax, 64, 657-663. doi:10.1136/thx.2008.1093899. Downs, S., Schindler, C., Liu, S., Keidel, D., Bayer-Oglesby, L., Brutsche, M.,… SAPALDIA Team (2007). Reduced exposure to PM10 and attenuated age-related decline in lung function. The New England Journal of Medicine, 357(23), 2338-2347. doi:10.1056/NEJMoa07362510. Morsch, A.L., Amorim, M. M., Barbieri, A., Santoro, L. L., & Fernandes, A.L. (2008). Influence of oscillating positive expiratory pressure and the forced expiratory technique on sputum cell counts and quantity ofinduced sputum in patients with asthma or chronic obstructive pulmonary disease. Jornal Brasileiro De Pneumologia : Publicacao Oficial Da Sociedade Brasileira De Pneumologia E Tisilogia, 34 (12), 1026-32.
Each year on May 30, the world unites to recognise World MS Day – a powerful movement that brings together the global Multiple Sclerosis (MS)
Asthma is more common than many people realise — affecting over 262 million individuals around the world. Yet despite how many lives it touches, asthma
In the pursuit of optimal respiratory health, understanding and implementing techniques like Chest Percussion can be a game-changer. This method, designed to enhance lung function
AirPhysio may be able to help by assisting with
✅Clearing the mucus clogging airways
✅Helps Promote Optimal Lung Capacity
✅Helps Promote Optimal Lung Hygiene
✅Helps treat Respiratory Conditions
✅May Reduce the chance of developing lung infections
✅Recommended by doctors, physical Therapists & Pulmonologists
✅Helps Make Breathing Easier
✅Sold in 106 countries globally


Do you suffer from Dry or Persistent Cough, Breathlessness, Respiratory or Severe Respiratory Conditions, or Shortness of Breath as you Get Older?

THIS PRODUCT MAY NOT BE RIGHT FOR YOU. READ THE WARNINGS BEFORE PURCHASE (Contraindications of Untreated pneumothorax; Tuberculosis; Oesophageal surgery; Right-sided heart failure; Middle ear pathology, such as ruptured tympanic membrane)
FOLLOW THE DIRECTIONS FOR USE
IF SYMPTOMS PERSIST, TALK TO YOUR HEALTH PROFESSIONAL

Gallery
AirPhysio is an Oscillating Positive Expiratory Pressure (OPEP) device that is used for mucus clearance and lung expansion to help in the treatment of respiratory conditions. The use of the AirPhysio device helps to facilitate secretion mobilization and maximize lung volume for cleaner healthier lungs.
© AirPhysio 2022 – All Rights Reserved
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |